Tip Cards
Clinical Documentation Integrity (CDI)
Tip Card- TEAM Guide Transforming Episode Accountability Model
Tip Cards
Clinical Documentation Integrity (CDI)
Webinars
Trauma Registry
This session focused on abdominal gunshot wounds, led by our Trauma Quality Director, Michael Trelow, with special guest surgeon Dr. Christine Toevs, who will share her clinical insights.
Session Highlights:
A great opportunity for trauma registrars to sharpen skills and strengthen data accuracy!
Webinars
Trauma Registry
Catch Trauma Quality Director Michael Trelow’s session on how the Trauma Registry supports stronger performance improvement.
You’ll learn how to:
Take your expertise in trauma performance improvement to the next level with tips you can implement immediately in your quality and registry workflows.
Blogs
Health Information Management & Coding
Accurate ICD-10-PCS revision total knee arthroplasty coding is critical for compliance, reimbursement, and audit defense. However, revision knee cases, especially partial component exchanges, remain one of the most misunderstood and highly scrutinized areas in inpatient coding. Coders often struggle to determine whether a procedure should be reported using the Revision root operation or coded as a combination of Removal and Replacement.
This blog walks through a real-world clinical scenario involving a revision of a tibial component only. Using official ICD-10-PCS guidelines and best practices, we explain correct diagnosis selection, procedure coding, sequencing, and DRG impact. By the end, you will have a clear, practical framework to confidently code with similar encounters while reducing compliance risk.
A 79-year-old male is admitted for worsening pain and instability of a right total knee replacement that was originally performed six years ago. Imaging confirms mechanical loosening of the tibial component without evidence of infection.
During surgery:
The correct principal diagnosis is:
Although the surgeon uses the term “revision” in the operative note, ICD-10-PCS coding is based on what was done, not the procedure name. According to ICD-10-PCS guidelines, the Revision root operation is reserved for procedures that correct or adjust a device without removing it, such as repositioning or tightening.
In this case, the failed tibial component was completely removed and replaced.
Therefore, the correct approach is to code:
Together, these two codes fully and accurately describe the procedure performed.
Correct DRG Grouping- When coded correctly, this encounter groups to:
Misclassifying a partial revision as a full joint replacement or failing to code device removal can trigger payer audits, recoupments, and compliance exposure. Revision arthroplasty cases are consistently high-risk for denials.
To support compliant ICD-10-PCS revision total knee arthroplasty coding, coders and auditors should always:
Additionally, documentation must clearly support medical necessities, such as mechanical loosening, instability, or device failure. If infection is present, coding and DRG assignment change significantly and may introduce a major complication or comorbidity.
For further guidance, refer to official resources from the Centers for Medicare & Medicaid Services and the American Hospital Association.
Accurate ICD-10-PCS coding for revision knee arthroplasty requires careful document review, strong understanding of root operations, and adherence to official guidelines. Coding partial knee revisions correctly helps protect reimbursement and reduces compliance and audit risk.
Need help reviewing complex orthopedic cases or training your coding team?
Contact us today and learn how to code ICD-10-PCS revision total knee arthroplasty correctly, avoid denials, and ensure compliance with this step-by-step guide.
Webinars
Trauma Registry
Missed our recent webinar? You can now watch the full recording of “2026 NTDS Updates: Get Ready for the 2026 Dictionary.”
Led by our expert, Michael Trelow, this session walks you through the most important changes coming to the 2026 NTDS Dictionary.
In the recording, you’ll learn how to:
Whether you work in trauma registry, coding, data abstraction, or clinical workflow support, this recording will help you prepare for the upcoming updates with clarity and confidence.
Webinars
Trauma Registry
After the presentation, participants will be able to:
Date: January 28th
Time: 12:00 PM EST
Blogs
Clinical Documentation Integrity (CDI)
It is the responsibility of the Trauma Registry Professional to be familiar with each hospital event to accurately identify and document the correct data points. Since hospital events can change from year to year, the Trauma Registry Professional must be adaptable to keep up with these changes.
Everyone has their own learning style. Some people grasp the NTDS document by reading it directly, while others find it more helpful to use an algorithm. Some key points to be aware of include learning how to correctly read the NTDS and reviewing the 2024 Hospital Event Algorithm flow chart. This is available for download from AKI TEST (facs.org). For the 2025 NTDS, the algorithms are integrated into the documentation.
When reviewing hospital events, extra effort is needed to identify specific conditions, such as Acute Kidney Injury. To comprehend what you’re examining, you might need to broaden your knowledge by learning about factors like what defines an eGFR.
Acute Kidney Injury Example:
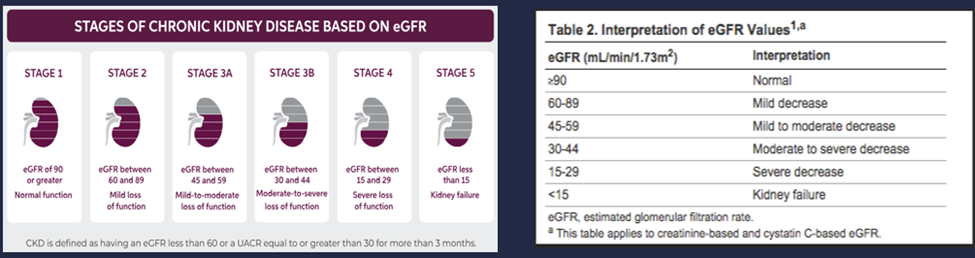
Chronic Kidney Disease in Type 2 Diabetes | Kerendia® (finerenone) | Patient Site (kerendia-us.com)
Understanding the language and structure of NTDS Hospital Event documentation is crucial for accurate data interpretation and reporting. The presence of “and/or” statements requires careful attention to ensure that the data is categorized correctly. Additionally, the flow of data within the algorithm can vary, highlighting the importance of a thorough review of each document. Familiarity with these nuances is essential for maintaining the integrity of the data and supporting effective patient care outcomes.
The American College of Surgeons Trauma Quality Improvement Program (ACS TQIP) plays a crucial role in enhancing patient care by collecting data on hospital events. This data is instrumental in identifying facilities with lower incidence rates, which can then serve as benchmarks for others. By analyzing and adopting the strategies of these leading facilities, hospitals can work towards reducing their own event rates, ultimately improving patient outcomes and elevating the standard of trauma care.
Blogs
Utilization Management & Case Management
As acute care case managers, we face numerous challenges in ensuring patients receive optimal care and effective discharge planning. This blog highlights these barriers and offers resolutions and advice to overcome them. Many challenges are interconnected, often compounding one another, making it critical to approach them with a strategic mindset.
In the complex healthcare landscape, case managers play a pivotal role in ensuring seamless patient care transitions, particularly as patients prepare for discharge from the hospital. These professionals juggle multiple responsibilities, including patient advocacy and resource management, to navigate the intricacies of care coordination.
Below, we explore five key challenges faced by case managers, specifically discharge planners in acute care settings, along with practical solutions to address them effectively.
Studies from the Journal of the American Medical Association reveal that nearly half of Medicare beneficiaries have at least three chronic conditions, making them more medically complex patients. Coordinating care for these patients requires collaboration among various specialists—physical therapists, hospitalists, dietitians, pharmacists, and behavioral health providers, among others.
Coupled with staffing shortages, budget constraints, and limited availability of post-acute services, case managers often struggle to deliver optimal care and discharge planning.
The American Association of Colleges of Nursing reported the largest drop in hospital-employed nurses in four decades from 2020 to 2021. These shortages lead to heavier caseloads for case managers and the need to onboard inexperienced staff, which can impact the quality and continuity of care.
Case managers face high levels of stress due to the urgency and complexity of their roles. Constant interruptions, emotional labor, and the need to juggle priorities can lead to compassion fatigue and burnout.
Case managers must ensure safe, effective discharges while adhering to strict regulatory requirements. Frequent changes in federal regulations, public health policies, and payer guidelines add to the complexity.
Strong communication is essential for case managers to coordinate care effectively. Challenges include language barriers, cultural differences, and cognitive or emotional factors affecting patients and families.
Addressing challenges in case management requires interdisciplinary collaboration, adaptable workflows, and supportive technology to streamline communication and resource allocation. By prioritizing education, team support, and proactive problem-solving, case managers can improve outcomes for patients and families alike.
https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/213908
https://www.aacnnursing.org/news-data/fact-sheets/nursing-shortage
Blogs
Trauma Registry
Sometimes, the need for a massive transfusion in trauma patients is immediately apparent when they arrive in the emergency department trauma room. However, occasionally, a seemingly stable trauma patient may suddenly experience a drop in blood pressure, surprising the trauma team.
In the trauma data world, trauma registry professionals must come to know predictive tools that they must be able to document accurately. Such predictive tools would include Revised Trauma Score (RTS), Injury Severity Score (ISS), Glasgow Coma Scale (GCS). We are going to look at another predictive tool, Shock Index (SI) and break it down in what it is predicting.
Shock Index defined
Blood pressure and heart rate, when used individually, fail to accurately predict the severity of hypovolemia and shock in major trauma. The Shock Index (SI) is a straightforward calculation, derived by dividing the heart rate (HR) by the systolic blood pressure (SBP). This index can be quickly determined by Emergency Medical Services (EMS) and is valuable in assessing whether a patient needs transport to a trauma center. Additionally, in the Emergency Department triage area, SI helps identify patients at risk of hemorrhagic shock (HS) and the potential need for massive transfusions. It has been researched in patients who are either at risk of or experiencing shock due to various causes, including trauma, hemorrhage, myocardial infarction, pulmonary embolism, sepsis, and ruptured ectopic pregnancy.
Shock Index Levels
When it is broken down, the SI is looking at different levels of shock:
Trauma Registry professionals should be able to understand all the predictive tools and help them know the SI and to not simply add it to the trauma registry should the trauma center be collecting the data but be able to know that the higher the SI, be looking for use of the massive transfusion policy (MTP) and find the type and number of units of different blood products being used. Being able to link their critical thinking to potential performance improvement issues will make the trauma registry professional stand out and aid in better care for the trauma patient.
To read more about the SI, in 2010 the paper was presented at the 23rd Annual Scientific Assembly of the Eastern Association for the Surgery of Trauma:
“Identifying Risk for Massive Transfusion in the Relatively Normotensive Patient: Utility of the Prehospital Shock Index”
*Vandromme, M. J., Griffin, R. L., Kerby, J. D., McGwin, G., Jr, Rue, L. W., 3rd, & Weinberg, J. A. (2011). Identifying risk for massive transfusion in the relatively normotensive patient: utility of the prehospital shock index. The Journal of trauma, 70(2), 384–390. https://doi.org/10.1097/TA.0b013e3182095a0a
Blogs
Trauma Registry
There has been considerable discussion in trauma centers about the optimal number of charts a Trauma Registry Professional should close daily. Some hospitals impose high demands, leading to rapid turnover among registrars. While tracking productivity is essential, it’s crucial to balance the number of charts closed daily with the complexity of data points that need to be abstracted and entered, along with other duties they are asked to perform.
The primary role of a Trauma Registry Professional involves abstracting data from electronic health records (EHR), accurately entering this information into the hospital’s trauma registry, and adhering to national coding standards from the National Trauma Data Standard (NTDS) and other relevant courses like AIS courses. Trauma Registry Professionals must be well-versed in the NTDS data dictionary and may also need to follow additional state-specific data requirements. Additionally, they might have to abstract certain local hospital data points that programs want to track.
According to the American College of Surgeons’ 2022 Standards Resources for the Optimal Care of the Injured Patient, each trauma center must have at least 0.5 FTE dedicated to the trauma registry per 200–300 annual patient entries. The count of entries is defined as all patients who meet NTDS inclusion criteria, and those patients who meet inclusion criteria for hospital, local, regional, and state purposes.” Trauma program managers and directors all know this requirement.
It is in the Additional Information that the ACS adds, “Trauma centers must take into account the additional tasks, beyond the abstraction and entry of patient data, that are assigned to the registrar. Processes such as report generation, data analysis, research assistance, and meeting various submission requirements will decrease the amount of time dedicated to the meticulous collection of patient data. Electronic downloads into the trauma registry also create additional tasks, as does ongoing data validation before data acceptance. Additional staff will be required to perform these tasks to ensure the integrity and quality of registry data, which are used for prevention, PIPS, and other essential aspects of the trauma program.”
Is the additional information being included when the trauma service decides to put a charts per day number in place? Let’s remember that not everyone works at the same pace. Are those differences accounted for? Chances are the current TPM has not hired or supervised all the registrars since the trauma service was started. The registrars that are in place now are often products of another TPM. Some registrars are fast in how they abstract charts, some are more deliberate, making sure they capture everything, and some decide to chase every rabbit that presents itself, thus making them a lot slower. Accuracy and consistency are paramount, and productivity should be tracked alongside accuracy. Data validation parameters should be in place, and registrars should be evaluated based on their experience and certifications. Balancing the number of charts closed daily with data accuracy is crucial.
The 2022 Standards, item 6.1, requires all trauma centers to have a written data quality plan with at least quarterly reviews. Data validation is key to maintaining quality data. Sharing data validation results in a shared folder allows the TPM and Trauma Surgeon to monitor staff accuracy continuously. To begin the process of productivity, you need to obtain some data from the trauma registry. Run several reports that would show average ISS, average Hospital Days, and average ICU days. This baseline will help to be a determining factor in the productivity process.
A simple way to track productivity is to use an Excel sheet that Trauma Registry Professionals can update weekly and submit to the TPM. The sheet should include the following information:
By tracking the number of charts completed and the time spent on each, registrars can gain a clear understanding of their productivity. Without this data, both the registrar and the TPM lack insight into actual performance levels. This tracking system allows registrars to monitor their improvement over time, fostering a sense of increased productivity.
Once you have this data, you can determine a reasonable daily chart closure target that your staff can manage accurately. Productivity and accuracy should be the primary goals for each registrar. This approach will also help you justify the need for additional staff to the administration, especially in response to any increases in trauma cases, as you’ll have a clear understanding of the workload capacity.
Resources for Optimal Care of the Injured Patient | ACS (facs.org)
Blogs
Cancer Registry
“Leaders become great, not because of their power, but because of their ability to empower others.” – John Maxwell.
Cancer registry leaders are pivotal to the success of the oncology service line. Their role is not only to lead the registry team but also to manage registry data effectively. Strong leadership and management in cancer registries ultimately enhance the care received by each cancer patient and improve the quality of data that drives advancements in cancer care.
7 Principles for Success as a Cancer Registry Leader:
Successful leaders share several traits regardless of industry:
These traits enhance team productivity and accuracy, increase morale and staff retention, and improve the accuracy and reliability of registry data.
Essential Leadership Skills for Cancer Registry Managers:
Communication
Motivation and Engagement:
Problem-Solving:
Decision-Making:
Managing Cancer Registry Data
You are an interpreter, translator, and data manager as a cancer registry manager. When data is requested, take the time to understand what information is being sought. Your stakeholders, executives, and researchers may not fully articulate their needs. By understanding their goals, you can provide impactful data. Always provide a concise written summary that answers their questions and offers an interpretation of the data. Thoroughly review your data before sharing and address accuracy and workflow issues with your team.
3 Key Data Management Principles:
Empowering Your Team
As a leader in the Cancer Registry, it is imperative to empower your team. You are the department visionary, expert, and servant. Creating a specific cancer registry vision that aligns with your organization will inspire and motivate your team. Elevate your emotional intelligence and ensure you are building positive relationships. Communication and empathy are vital. Successful leaders are servants—your position is to serve your team.
Empower Your Team Through:
Training and Development:
Delegation:
Feedback and Recognition:
3 Key People-Focused Leadership Strategies:
Feedback and Continuous Improvement
Effective leadership involves creating feedback loops where you can continuously give and receive feedback to improve. Avoid creating loops of only constructive criticism. Aggressive, demeaning, and highly critical leaders lead to stagnant teams, low productivity, low morale, and low retention.
Various methods can propel your team forward and improve data collection in the cancer registry. Implement one strategy at a time. Remember, we are not just capturing data; we are telling each patient’s cancer story in a statistically significant way that translates data into meaningful outcome improvements and programmatic developments.
Leading with excellence in the cancer registry involves managing data with precision and empowering your team to achieve their best. You can create a thriving, productive environment that improves cancer care and registry data quality by focusing on data integrity, standardization, usability, and people-focused leadership.
Embrace these principles and watch your team and the data they manage reach new heights of success.
Blogs
Trauma Registry
Critical thinking skills are highly sought after today and are actively taught. With the constant influx of information from TV news and the Internet, it’s crucial to develop critical thinking skills to discern the truth. This is especially vital for Trauma Registry Professionals who handle abstracted information and processes within trauma services.
Critical thinking is defined as the “objective analysis and evaluation of an issue to form a judgment.” Key terms in this definition include objective analysis, evaluation, and judgment, which are essential components of the process. Critical thinking fosters effective problem-solving and creativity, and it underpins rational decision-making.
Below are realistic examples of how critical thinking resolved an issue for trauma registry professionals. The process of critical thinking involves five distinct phases.
5 Phases of Critical Thinking
By employing critical thinking techniques, the trauma service was able to quickly obtain EMS trip sheets. Initially, when the trauma service began distributing custom reports, it took some time for EMS agencies to recognize their value. However, once they did, they eagerly incorporated the reports into their performance improvement processes.
Over time, EMS agencies began contacting the Trauma Registry Professionals within 24 hours of patient drop-off to inquire about their reports. If they hadn’t left a trip sheet, the registrar would inform them, and the EMS agency would promptly send it over within five minutes. This change significantly reduced the time the Trauma Registry Professional spent on Mondays calling for trip sheets, from up to four hours to just 30 minutes. As a result, the trauma service received the trip sheets immediately and could promptly deliver reports back to the EMS agencies, enhancing communication between the two parties.
While no one is perfect at critical thinking, consistent practice offers a significant advantage. Strong critical thinking skills enable us to understand ourselves and our opinions better, and to examine diverse perspectives without fear or bias. These skills are invaluable tools for proactively addressing problems in both personal and professional contexts.
Blogs
Trauma Registry
First and foremost, data validation is an educational tool that sharpens the skills of the Trauma Registry Professional and in turn, develops better data for the trauma centers to use to improve patient care. Data validation highlights areas of weakness and motivates the registrar to pursue additional training, ensuring the accuracy of data points
There are many ways to do data validation on the trauma registry, so there are multiple tools that one can find to fit their trauma center needs. The main goal is to train the Trauma Registry Professionals to get the most accurate data from the EHR to the registry.
The Guidelines:
The National Trauma Data Standard (NTDS) serves as the essential data dictionary for all trauma registrars. It details all required data fields, providing definitions, element values, and additional information to ensure correct data entry. The NTDS includes a data source hierarchy guide, directing registrars to the appropriate documents for data retrieval. It also outlines associated edit checks, specifying that Level 1 and 2 edit checks must be corrected before data can be uploaded to the National Trauma Data Bank (NTDB). Statewide trauma data dictionaries, for states that track additional data, adhere to the same format as the NTDS.
Hospital-based data dictionaries are designed to indicate where to obtain data from the EHR. They should include an additional column specifying the exact location in the EHR to pull the data. This will assist new registrars in accurately entering data into the trauma registry.
According to the American College of Surgeons (ACS), up to 10% of the total charts per month must be validated. There are two schools in data validation of the trauma registry:
If you select 20-25 data points and your registrars consistently achieves 100% accuracy, you can replace one of those data points with a new one to maintain engagement. Trauma Registry Professionals are aware of the data points being monitored, which helps ensure their integrity.
One method to do data validation is that you have the data analyst and Trauma Registry Professional and PI RN, or other trauma registrar in the same room. The data analyst gives a registry number to the Trauma Registry Professional who in turn tells the PI RN the medical record number. After the PI RN opens the EHR, the analyst then goes through each data point that is being tracked. The PI RN finds it in the medical record, then answers the question and the Trauma registry Professional has to either acknowledge it as correct, or say it was missed in the registry. Then they can discuss where the registrar found the data.
In data validation, you aim to identify patterns of missed or incorrect data. If a pattern is detected, you can guide the registrar to relevant courses to improve their understanding. Options include trauma registrar courses, ICD-10 courses, and AIS courses. Sharing validation scores on a shared drive allows the Trauma Program Manager and Trauma Medical Director to quickly review the inter-rater reliability (IRR) of the trauma registrars, ensuring high-quality reports from the registry.
In conclusion there are many ways to validate a record for the Trauma Registry Professional. The main point is to be educational because no one is perfect. It should be a two-way street where the reviewer identifies the missing/incorrect data, presents it to the registrar and the registrar can show the reviewer where they got the data. All of this is done to help the registrar abstract and enter high quality data to help the hospitals improve the treatment of the injured patient.